Breathing by Breas
Comfortable ventilation with excellent monitoring capabilities
Our mission is to improve the quality of life and care of respiratory patients around the world through a personal commitment to innovation, quality, and customer focus.
Travel Sized CPAP
The compact design makes it easy to bring the Z2 Auto with you at any time
Education
On the Education by Breas website we share knowledge and best practices in respiratory care
News
Read our latest press releases and content.
Highlights
October 17, 2023
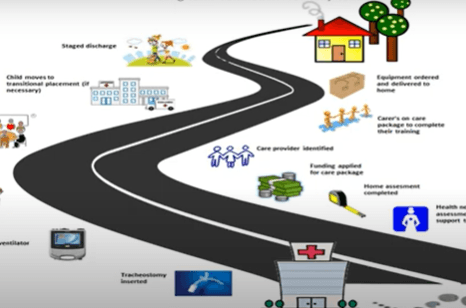
Webinar video: Transitioning a Child Home With a Ventilator
October 17, 2023
Webinar video: Transitioning a Child Home With a Ventilator

August 15, 2023
Webinar video: Breas Lecture Syndrome de Déventilation
August 15, 2023
Webinar video: Breas Lecture Syndrome de Déventilation

August 9, 2023
Webinar video: When to Withdraw HMV? Experience End of Life
August 9, 2023
Webinar video: When to Withdraw HMV? Experience End of Life

July 25, 2023
Webinar video: The Role of Nebulization & Humidification for Airway Clearance
July 25, 2023